Patient Information
General Patient Information
The Diagnostic Endoscopy Centre participates in audits and data verification to ensure we are compliant with and maintaining the highest standards of clinical practice in relation to your care.
In order to participate we may be required to use patient records or data for verification purposes (an example of this is during the accreditation process with the Australian Council on Health Care Standards, surveyors may wish to confirm documentation or follow the care pathway to ensure standards have been met) and we will always de-identify the record prior to granting access. Where we are unable to de-identify a patient record we will contact your personally to request your permission to grant access to your information.
If you have any further queries about circumstances where the Diagnostic Endoscopy Centre may release information contained in your medical records please contact the Chief Executive Officer on 8382 6622 or jan@endoscopy.stvincents.com.au.

Things To Know Before The Endoscopy Procedure
- Please read ALL information given to you carefully and as soon as possible.
- Follow the bowel preparation instructions given to you.
- Arrange for a responsible adult to collect you. For your safety you will NOT be permitted to leave the Unit unescorted, in a taxi unaccompanied or to drive a car for the rest of the day. Cancellation of your procedure may take place if these arrangements are not made. You can expect to be at the DEC for approximately 2-3 hours. Please note this Unit closes at 6.30pm Monday to Thursday and 6pm on Friday and you will need to arrange for your escort to collect before this time.
- It is advisable to wear loose, comfortable clothing and non-slip shoes.
- Please complete the Booking Information Form, Care Pathway where instructed and provide a list of your medications and return to us as soon as possible. If you are unable to ensure these documents reach us before your appointment, please bring them with you on the day. You must also bring your referral letter, Medicare card, Pension Card and/or Veteran Affairs Card (if applicable).
- All excesses and co-payments are payable on the day of admission.
- Please do not bring valuables.
- A medical certificate will be issued if required.
Medications
Recovery: 8382 6615
Prior to any sedation it is desirable that you are as healthy as possible. This is why we advise you to take certain medications as normal prior to your appointment, especially if you have high blood pressure, heart problems, epilepsy, or any other medical conditions. There are some exceptions to this rule. Please read the following information carefully.
- Iron tablets should be stopped 5 days prior to your colonoscopy.
- Anti-inflammatory drugs should be stopped 5 days prior to your procedure.
- Blood thinning tablets (anti-coagulants) may need to be stopped as directed, please obtain medical advice prior to ceasing these medications. You may not be able to stop taking them and if that is the case we need to be aware you have continued to take them.
- Diabetic medications (insulin or oral tablets) generally should be withheld on the morning of the procedure. Please discuss with your Doctor. Please bring any diabetic medications with you on the day of admission. Your blood sugar level will be recorded on admission and again after your procedure. If you are taking any of the following diabetic medication (Forxiga, Jardiance, Xigduo, Jardiamet, Steglatro or Segluromet) they should be ceased 3 days prior to your procedure.
- Weight loss medication (e.g. Ozempic, Semaglutide, Rybelus, Tirzepatide, Monjaro, Dulaglutide, Trulicity, Liraglutide, Saxenda) should be stopped prior to your procedure. If you are on a weekly injection or tablet, you must not administer your dose 7 days prior to your procedure. If you are on a daily injection or tablet, do not administer your dose the day prior to your procedure or the day of your procedure.


Preparation For Colonoscopy
To enable a thorough and safe examination, the colon will need to be completely cleansed at home by the use of laxatives and the drinking of a quantity of flavoured solution, which passes through without upsetting your body. Please refer to your preparation instructions for specific details of which preparation to use and when to take each dose. As you may need to use the bathroom during the night please be aware this represents a falls risk to you. Please take the necessary steps in your home to improve your safety.
Special Considerations
Please make nursing and clinical staff aware of any allergies. If there is any chance you may be pregnant please let our staff know.
Consent For The Removal Of Polyps
It will not be possible to discuss the removal of your polyps with you at the time of examination, as you will be sedated. Therefore your consent for the removal of polyps will be obtained during the consent process with your treating Endoscopist. If you have any queries or reservations, please inform the admission sister or the treating Endoscopist.
Sedation and Anaesthetics
If you would like to know more information about sedation and the agents used in our procedures, please visit the following websites: Australian Society of Anaesthetists (ASA) and Australian and New Zealand College of Anaesthetists (ANZCA)
Consultation Fees
The Diagnostic Endoscopy Centre is a private medical practice. Consultations are billed at private patient rates and fees are payable on the day.
Fees are payable on the day of consultation and we accept EFTPOS, Mastercard, Visa and American Express. We are able to submit your claim to Medicare on your behalf if you have registered with Medicare for this service. If you have not registered, you will need to claim your rebate yourself by providing Medicare with your invoice and receipt.
Concessions
Holders of a current Australian Government issued Aged Pension Card may be offered a discounted consultation fee provided that the entitlement card is produced at the time of consultation. Holders of Department of Veterans Affairs gold cards will be bulk billed.
If you are experiencing financial difficulty please discuss this with your doctor at the time of consultation. Reception staff are not permitted to alter billing unless directed to do so by the doctor.

Frequently Asked Questions
Find out the answers to Diagnostic Endoscopy Centre’s most frequently asked questions
- A referral from your GP
- Your insurance information
- Any recent blood test results or imaging reports
- A completed Medical History form ( if you have not already returned one to us)
- A list of the current medications you are taking including any known medication allergies
Please allow 2 – 3 hours from the time you arrive at the clinic. Procedure times can vary from patient to patient.
Your clinician will see you before you are discharged to discuss the findings of your test and to organise and follow up appointments if required.
The IV sedation given during your test can affect your judgement and reflexes. It is for this reason that you will be considered legally impaired and are not permitted to drive for a minimum of 12 hours after having your procedure. For your safety you must have a responsible adult come to the clinic and escort you home.
You cannot catch public transport home unless you are accompanied by a responsible adult. This is for your safety and that of fellow travellers.
We advise that you keep the day of your procedure free to recover. You must not drive a motor vehicle, operate any form of machinery or make any important decisions for the rest of the day. You should be fine to resume normal activities including work and exercise by the following day.
Yes, the admitting nurse will ask if either you or your carer requires a medical certificate for the day of your procedure. This will be given to you on discharge from the clinic.
- Loose, comfortable clothing and non-slip shoes
- Make-up should be kept to a minimum. Excess eye makeup can cause irritation to the eyes.
- Valuables including jewellery should be left at home. We do not accept any responsibility for loss or damage of your valuables.
The Diagnostic Endoscopy Centre has contractual arrangements with most health funds for accommodation and theatre fees.
Hospital Provider Agreements
The DEC has contractual arrangements with the majority of private health funds* for accommodation and theatre fees (hospital fees). Provided you are a financial member of one of these funds or your fund belongs to AHSA, have private hospital cover, and you have served all your mandatory waiting periods and you do not have an annual excess or co-payment, you will have no out of pocket expenses under our contract conditions. Please feel free to contact our staff who will supply you with the necessary information regarding your treatment to enable you to confirm your level of coverage with your Health fund. We are able to check the financial status of patients who are insured with HCF, Medibank Private, NIB, Teachers Federation, Manchester Unity, Australian Unity (just to name a few) via the MBF website, the HAMBS website and access to the THELMA website and we will provide you with informed financial consent prior to undergoing any treatment with us.
[* Please contact our friendly reception staff to confirm if your health fund is covered by our health fund contracts.]
Our doctors participate in the known gap scheme for their private procedure fees. Our reception staff will advise you of any gaps payable by you on admission. Gap payments for doctor fees are not refundable from your health fund.
Patients who hold Department of Veteran Affairs gold cards will also be fully covered whilst at the DEC. Prior approval must be obtained from Department of Veteran Affairs for all white cardholders.
Our Reception and Accounts staff are available during business hours, Monday to Friday, to assist you with any queries regarding your Health fund or our accounts.
Accounts: (02) 8382 6627
Reception: (02) 8382 6622


Pathology Accounts
Please be advised, you may have biopsies (pathology) taken during your procedure and an external pathology company will process these specimens. The accounts for these services are generated by the pathology company.
Generally due to the scope of biopsies and tests requested it is not possible to give an estimate of the charges for these services.
As this service is the result of an inpatient treatment, the accounts are claimable from Medicare and your private health fund (if applicable). Some companies provide these services as “no-gap” but we are not in a position to request this service from the pathology provider.
Anaesthetic Accounts
Anaesthetic accounts will also be raised on the day of treatment by the anaesthetist who will assist your doctor.
As inpatient treatment, this account is claimable from Medicare and your private health fund (if applicable).
Many of our anaesthetic staff participate in the “no-gap” billing schemes and in these cases your accounts for anaesthetic services will be forwarded directly to your health fund.
Patient Care
We would like to make your visit with us as comfortable as possible.
Your health and well-being are our primary concern.
We would like to make your visit with us as comfortable as possible. Your health and well-being are our primary concern.
The Diagnostic Endoscopy Centre was established in 1990 with the sole purpose of providing the highest quality health care in Endoscopy. Our commitment continues to strengthen and this is reinforced by our ongoing accreditation status with the Australian Council of Healthcare Standards ensuring we achieve the highest possible standard in health care and quality.
We are licensed as a Day Hospital with the Ministry of Health NSW. We have Hospital Purchaser Provider Agreements (contracts) with most of the major health funds to maximise patient benefits.
Are There Risks Involved?
As with any medical procedure complications are possible although rare. That is why all clinicians associated with the DEC are fully qualified specialists in their respective fields – gastroenterologists, surgeons, anaesthetists and registered nurses. Your doctor will discuss the specific risks prior to your treatment.
Maintenance and surveillance of the highest possible standards in cleaning and disinfection of equipment following stringent infection control guidelines avoid potential transmission of disease, particularly Hepatitis B, C and AIDS. As with any medical procedure complications are possible although rare. That is why all clinicians associated with the DEC are fully qualified specialists in their respective fields – gastroenterologists, surgeons, anaesthetists and registered nurses. Your doctor will discuss the specific risks prior to your treatment.
Maintenance and surveillance of the highest possible standards in cleaning and disinfection of equipment following stringent infection control guidelines avoid potential transmission of disease, particularly Hepatitis B, C and AIDS.
Patient Rights
You have the right to:
- An environment that is safe and respects privacy and confidentiality
- To be treated with courtesy and to have your ethnic, cultural and religious practices and beliefs recognised
- An environment that promotes each patient’s sense of personal worth and well-being
- A clear, concise and understandable explanation of:
- Your condition or problem
- Your planned investigation and
- Any possible after effects and side effects and any serious risks involved
- To be informed of and give consent to any procedure where consent is required by law. By entering the DEC it is our understanding that you are requesting treatment
- Seek a second opinion
- To know the identity and professional status of any doctor and staff caring for you
- Prior to the commencement of your procedure an explanation of all costs
- The right to have details of your condition and treatment kept confidential by medical and all other staff at the DEC, unless the law requires that said information be given to the authorities
These rights are consistent with the current national charter of healthcare rights (March 2013).
Patient Responsibilities
It is your responsibility to:
- Be as accurate and as honest as possible in providing information about your health in order to plan your appropriate treatment
- Accepting responsibility for your decisions if you refuse medical treatment
- Be considerate of the needs and rights of other patients and staff at the DEC
- Keep appointments as scheduled
- Accept responsibility for payment of all fees generated in your name as a result of your treatment with us
If you wish to express a concern about any aspects of your care you may to so by informing any staff member. Your concern will be given immediate attention. At all times our focus is your care, safety and well-being
 Antimicrobial Stewardship
Antimicrobial Stewardship
Antimicrobial stewardship involves making sure antibiotics are used wisely. Bacteria can develop resistance to specific antibiotics, meaning that the antibiotic is no longer effective against the same bacteria.
To help prevent the development of current and future bacterial resistance,
it is important to prescribe antibiotics according to the principles of antimicrobial stewardship, such as prescribing antibiotics only when needed (and not for mild infections such as colds, earache or sore throats).
This Clinical Care Standard tells you what care may be offered if you have an infection that needs antibiotics. You can use this information to help you and/or your carer make informed decisions, in partnership with your health professional.
UNDER THIS CLINICAL CARE STANDARD

A patient with a life-threatening condition due to a suspected bacterial infection receives prompt antibiotic treatment without waiting for the results of investigations.
This Clinical Care Standard tells you what care may be offered if you have an infection that needs antibiotics. You can use this information to help you and/or your carer make informed decisions, in partnership with your health professional.
What this means for you: If you are extremely unwell with a suspected bacterial infection, you are given antibiotics as soon as possible.

A patient with a suspected bacterial infection has samples taken for microbiology testing as clinically indicated, preferably before starting antibiotic treatment.
What this means for you: Before you are prescribed antibiotics, samples may be taken to try to work out which antibiotic is the best to treat the infection. The samples may include blood tests, urine samples or wound swabs.
A patient with a suspected infection, and/or their carer, receives information on their health condition and treatment options in a format and language that they can understand
What this means for you: If you are thought to have a bacterial infection, your doctor or nurse discusses treatment options with you and/or your carer, which may or may not include giving you antibiotics.
When a patient is prescribed antibiotics, whether empirical or directed, this is done in accordance with the current version of the Therapeutic Guidelines (or local antibiotic formulary). This is also guided by the patient’s clinical condition and/or the results of microbiology testing
What this means for you: If you are prescribed an antibiotic, your doctor or nurse chooses which one, based on national or local recommendations. They should take into account any allergies and other health conditions you may have.
When a patient is prescribed antibiotics, information about when, how and for how long to take them, as well as potential side effects and a review plan, is discussed with the patient and/or their carer.
What this means for you: If you are prescribed antibiotics, your doctor or nurse discusses with you and/or your carer about when and how to take your antibiotics, how long to take them and any potential side effects. You may need to be seen again to review your progress.

When a patient is prescribed antibiotics, the reason, drug name, dose, route
of administration, intended duration and review plan is documented in the patient’s health record.
What this means for you: Your health record contains the details of your antibiotic treatment. This includes information on why you were prescribed antibiotics, the medicine name, the dose, how you take them (i.e. as tablets or an injection), how long to take them and any plans to review your treatment.

A patient who is treated with broad-spectrum antibiotics has the treatment reviewed and, if indicated, switched to treatment with a narrow-spectrum antibiotic. This is guided by the patient’s clinical condition and the results of microbiology tests.
What this means for you: If it is unclear which bacteria may be causing your infection, you may be prescribed an antibiotic that works against a wide range of bacteria (i.e. a broad‑spectrum antibiotic).
In this case, your doctor or nurse may order tests to review your progress and, on seeing the results, your treatment may change to a more specific antibiotic (i.e. a narrow‑spectrum antibiotic).
If investigations are conducted for a suspected bacterial infection, the responsible clinician reviews these results in a timely manner (within 24 hours of results being available) and antibiotic therapy is adjusted taking into account the patient’s clinical condition and investigation results.
What this means for you: If tests have been done to identify a suspected bacterial infection, your doctor or nurse reviews these results as soon as they are available (usually within 24 hours of being available). These results may lead to your antibiotic treatment changing or stopping.

If a patient having surgery requires prophylactic antibiotics, the prescription is made in accordance with the current Therapeutic Guidelines (or local antibiotic formulary), and takes into consideration the patient’s clinical condition.
What this means for you: Antibiotics may be given to you before surgery to reduce the risk of an infection after surgery. The prescription is also based on national or local recommendations.
More information on the Clinical Care Standards program is available from the Australian Commission on Safety and Quality in Health Care website at www.safetyandquality.gov.au/ccs.
Download a PDF version of this Consumer Fact Sheet: Antimicrobial Stewardship Consumer Fact Sheet
Cognitive Impairment Consumer Resources
The Australian Commission on Safety and Quality in Health Care has published a new consumer resource for people with cognitive impairment, their families and carers: My Healthcare Rights – a guide for people with cognitive impairment. The resource has been aligned with the Charter of Healthcare Rights and provides information about the care people with cognitive impairment can expect if they go to hospital. It was developed in collaboration with Dementia Australia, people living with dementia, and carers.
An additional version of this resource has been developed to make this important information about healthcare rights accessible to people with low English literacy living with cognitive impairment: About healthcare rights for people with cognitive impairment – Easy English Version.
The resource is also available in 10 community languages.
Australian Charter of Healthcare Rights – My Healthcare Rights
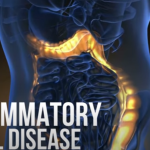
R.E.A.C.H out to us – Because together we make a great team